ALLERGIC RHINITIS (AR),DK JHA,MD
Sunday, May 25th, 2014INTRODUCTION
Allergic rhinitis is an inflammatory condition of nasal mucosa.
- It is a major chronic respiratory disease of children as it badly affects the quality of life and school performance of children
- It is most common chronic condition in children
- 20 -40% children of affluent societies suffer from this condition
- Its symptoms may appear in infancy and the diagnosis is generally established by the age of 6 years
- Risk factors include family history of atopy and serum IgE level more than 100 IU/ml before age 6 years.
- Up to 78% patients with asthma have AR and 38% of patients with AR have asthma.
Etiology
Two factors necessary for the development of AR are sensitivity to an allergen and the presence of allergen in the environment.
- Inhalant allergens are the main cause of AR.
- In India, spring season, February to April is flowering season of trees, in which so many pollens are in the air ,which is potent inhalant allergen.
- In temperate climates, trees pollinate in spring, grasses in early summer and weeds in late summer.
- In temperate climates, mold spores persists outdoor only in the summer and in warm climates, mold spores persist throughout the year.
- Other common allergens are dust mites,pet danders,and cockroaches.
CLINICAL MANIFESTATIONS:
Symptoms of pediatric allergic rhinitis include the following:
- Rhinorrhea
- Nasal congestion
- Postnasal drainage
- Repetitive sneezing
- Itching of the palate, nose, or eyes
- Snoring
- Frequent sore throats
- Constant clearing of the throat
- cough
- Headaches
- Epistaxis due to nose picking habits secondary to itching of nose
- Abnormal sleep pattern due to frequent awakening during night sleep secondary to nose block
CLINICAL SIGNS:
Allergic Salute
Allergic Shiner
Dennie Morgan Fold
Signs:
- Allergic salute
- Allergic shiners (dark, puffy, lower eyelids),
- Morgan-Dennie lines (lines under the lower eyelid),
- Transverse crease at lower third of nose secondary to allergic salute
- Allergic gape as the child keeps the mouth constantly open to breathe through it.
- Eyes: Marked erythema of palpebral conjunctivae and papillary hypertrophy of tarsal conjunctivae; chemosis of the conjunctivae, usually with a watery discharge; cataracts from severe rubbing secondary to itching
- Ears: Chronic infection or middle ear effusion
- Nose: Enlarged turbinates with pale-bluish mucosa due to edema; clear or white nasal discharge (rarely yellow or green); dried blood secondary to trauma from nose rubbing; rarely, polyps (if polyps detected on rhinoscopy, mandatory workup for cystic fibrosis in children)
- Throat: Discoloration of frontal incisors, high arched palate, and malocclusion associated with chronic mouth breathing (allergic gape); cobblestoning in the posterior pharynx ( Aggregation of lymphoid tissues which appears like cobblestones)secondary to chronic nasal congestion and postnasal drainage
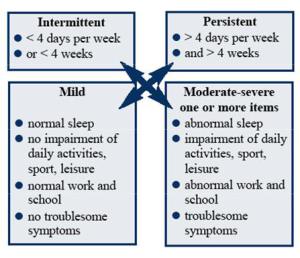
Classification based on severity of symptoms
This classification in accordance to ARIA guidelines(allergic rhinitis impact on asthma)has replaced the older classification of seasonal AR and perennial AR.
INVESTIGATION: Diagnosis is mainly clinical
- Skin prick test is the gold standard
- Total serum IgE indicate allergy to many allergens
- RAST(Radio-allegro-sorbent assay) indicate allery to specific allergen
- Blood eosinophilia may be helpful
- Eosinophils in nasal smear has good positive predictive value
- Imaging study may help but not mandatory
TREATMENT:
1 . Allergen avoidance– which is not possible all the time as the child may be allergic to so many allergens. Allergen proof bed and pillow coverings may reduce the exposure to mite allergen.Bed linen and blankets should be washed every week with hot water(>130dF).
2. Antihistaminics -this is the first line treatment mainly effective for mild intermittent AR, may be beneficial for moderate intermittent AR. Second generation antihistamines are preferred as they cause less sedation.
CETRIZINE:6months -24months: 2.5mg once daily in the evening
2-6years :2.5mg to 5mg once or twice daily
more than 6 years 5-10 mg once or twice daily.
LEVOCETRIZINE: 6-12 years:2.5mg once daily in the evening
more than 12 years: 5mg once daily in the evening
DESLORATADINE: -6months to 12months:1mg once daily
1 year to 5years:.1.25mg once daily
6years to 12years: 2.5mg once daily
more than12 years: 5mg once daily
FEXOFENADINE-2-11Years :30mg bd; 12 years and above 60mg bd or 180mg once daily
LORATADINE-2-5 Years 5mg once daily;>6 years 10mg once daily;more effective when given empty stomach
3. INTRANASAL CORTICOSTEROID-this is second line treatment for AR ,most effective to control all the symptoms and for maintenanc therapy.
MOMETASONE:recommended for 2years of age and above ,in the form of nasal spray,one spray (50mcg) into each nostril, once daily
FLUTICASONE: recommended for 4 years of age and above,in the form of nasal spray,one spray (50mcg) into each nostril,once daily.
BUDESONIDE:recommended for 6 years of age and above,in the form of nasal spray,one spray(100mcg) into each nostril,once daily.
TRIAMCENOLONE: recently FDA has approved its use for children 2 years of age and above,in the form of nasal spray,.one spray into each nostril ,once daily.
- Study has proved that there is no effect on growth of child after long term use.
- Troublesome adverse effect is epistaxis.
- Technique of taking it intranasally should be accurate for it to be effective.
Technique:
- make the child to sit comfortably and slightly lean forward
- ask him to blow the nose gently if possible
- block one nostril with index finger of your left hand
- shake the bottle well with your right hand
- hold the spray bottle upright with index finger and middle finger on either side off nozzle and thumb on the base
- insert the tip of nozzle into open nostril
- ask the child to inhale through open nostril
- as the child starts inhaling ,release the drug by suddenly pressuring over the base of nozzle
- ask him to exhale through mouth
- repeat the process on other side
4 Intranasal antihistamine: useful only for acute symtoms
- not well studied in children below 5 years of age
AZELASTINE:6-12 years:one spray(140mcg) into each nostril bd,
;more than 12 years :1-2 sprays into each nostril bd
5 Intranasal ipratropium:useful only for rhinorrhea
- not well studied in children below 5 years of age.
6 Monteleukast orally alone or in combination with antihistamine is effective for long term use
7 Immunotherapy:Indicated in children not well controlled with other medication or having toxic adverse effects with other medications.
- very effective in well chosen children
- not well studied in children beloe 5 years of age
8 Nasal irrigation with hypertonic saline is effective and inexpensive ;
9 Adrenergic agonist: Oxymetazoline-for symptomatic relief of nasal mucosal congestion
0.05% solution,instill 2-3 spray into each nostril twice daily
therapy should not exceed for more than 3 days
should not be repeated more than once a month
10.SLIT(sublingual immunotherapy) is a new modality: medicine is kept under tongue once daily
- Oralair(slit-medicine) has been recently approved by FDA for the age of 10 years and above: effective only if allergic to single aeroallergen
- Grastek is another SLIT medicine extracted from grass,recently approved by FDA for use in children 5 years of age and above
Bibliography
Akdis CA: New insights into mechanisms of immunoregulation in 2007. J Allergy Clin Immunol. 122:700-709 2008 19014761
Bousquet J, Khaltaev N, Cruz AA, et al.: Allergic rhinitis and its impact on asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2)LEN and AllerGen). Allergy. 63 (Suppl 86):8-160 2008 18331513
De Groot H, Brand PL, Fokkens WF, et al.: Allergic rhinoconjunctivitis in children. BMJ. 335:985-988 2007 17991980
Howath PH, Myginf N, Silkoff PE, et al.: Preface to outcome measures in allergic rhinitis. J Allergy Clin Immunol. 115:S387-S482 2005 15746879
Nelson HS: Allergen immunotherapy: where is it now?. J Allergy Clin Immunol. 119:769-779 2007 17337297
Radulovic S, Calderon MA, Wilson D, et al: Sublingual immunotherapy for allergic rhinitis, Cochrane Database Syst Rev (12)CD002893, 2010.
Simoens S, Laekeman G: Pharmacotherapy of allergic rhinitis: a pharmaco-economic approach. Allergy. 64:85-95 2009 19076532
Wahn W, Taber A, Kuna P, et al.: Efficacy and safety of 5-grass-pollen sublingual immunotherapy tablets in pediatric allergic rhinoconjunctivitis. J Allergy Clin Immunol. 123:160-166 2009 19046761
Wallace DV, Dykewicz MS, Bernstein DI, et al.: The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 122:S1-S84 2008 18662584
Weinstein S, Qaqundah P, Georges G, et al.: Efficacy and safety of triamcinolone acetonide aqueous nasal spray in children aged 2 to 5 yr with perennial allergic rhinitis: a randomized, double-blind, placebo-controlled study with an open label extension. Ann Allergy Asthma Immunol. 102:339-347 2009 19441606
Wright AL, Holberg CJ, Martinez FD, et al.: Epidemiology of physician-diagnosed allergic rhinitis in childhood. Pediatrics. 94:895-901 1994 7971008
Blaiss MS: Antihistamines: treatment selection criteria for pediatric seasonal allergic rhinitis. Allergy Asthma Proc. 26 (2):95-102 2005 15971466
Fireman P: Therapeutic approaches to allergic rhinitis: treating the child. J Allergy Clin Immunol. 105:S616-S621 2000 10856167
Garavello DW, DiBerardino F, Romagnoli M, et al.: Nasal rinsing with hypertonic solution: an adjunctive treatment for pediatric seasonal allergic rhinoconjunctivitis. Int Arch Allergy Immunol. 137 (4):310-314 2005 15970639
Gelfand EW: Pediatric allergic rhinitis: factors affecting treatment choice. Ear Nose Throat J. 84 (3):163-168 2005 15871585
Passali D: Consensus conference of allergic rhinitis in childhood. Allergy. 54:4-34 1999
Ressel GW: AHRQ releases review of treatments for allergic and nonallergic rhinitis. Am Family Phys. 66 (11):2164-2167 2002
Stone KD: Atopic diseases of childhood. Curr Opin Pediatr. 14:634-646 2002 12352260
Wallace DV, Dykewicz MS, Bernstein DI, et al.: The diagnosis and management of rhinitis: an updated practice parameter. J Allergy Clin Immunol. 122 (2 Suppl):S1-84 2008 18662584