RESISTANT TUBERCULOSIS IS NOT RARE IN CHILDREN,A CASE REPORT,DR.D.K.JHA MD
Jasmine is a 1o years female, came to me in OPD with her mother with complaint of cough for 20 days and occasional pain left side of chest for 5-7 days.Cough was sometimes dry and sometimes productive.There was no loss of appetite.Weight loss and fever was not noticeable by mother.Her father left the home 3 years back without information and mother is not knowing where he has gone.Mother told me that her father had tuberculosis of chest and he was taking treatment for that .On examination,she was cheerful,cooperative,thin built with weight of 22kg.Vitals were stable and there was no respiratory distress.On chest examination,breath sound was diminished over left infraclavicular,left mammary ,left infraaxillary and left interscapular regions.Percussion was not done as she was having pain in left side of chest.She was taking treatment for her symptoms from local physician with no relief.
Mother was carrying some investigations reports.Complete blood count was within normal limit.ESR was not raised.Mantoux test was done 4-5 days back but induration was not measured. I had measured the induration at first contact and it was 11mm,so I noted it positive.
She was also carrying a chest radiograph which was showing deviation of trachea towards left side with opacity in left upper lobe of lung.This radiograph may be passed as normal as done by some of my colleagues.
Sputum for AFB examination was done at their nearby DOTS centre and it was reported negative.
CHEST X-RAY PA VIEW
I thought ,the opacity in the left upper lobe of lung may be due to fibrosis of left upper lobe of lung which is not usually seen in children.My suspicion of fibrosis was due to deviation of trachea which, I was not able to explain by either pushing or pulling lung lesions other than fibrosis.There was no pleural effusion of either side,no pneumothorax of either side and no collapse of lung lobes of either side but there was a definite opacity of left upper lobe of lung. So I decided to go for a CECT chest
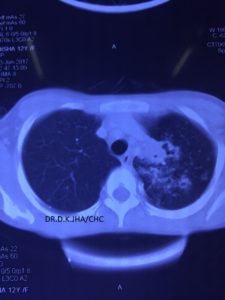
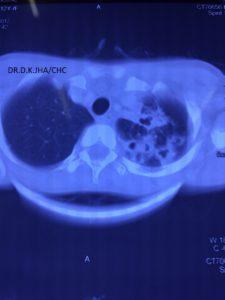
CECT CHEST
On viewing this CECT ches,t it was clear that there is fibrosis with nodular lesions in the left upper lobe.The CECT chest revealed more lesions.There was consolidation with areas of breakdown.
I did not give any treatment to the child and requested to collect sputum again.If not possible,it was explained to her that induced sputum and gastric aspirate will be collected and the process was described. The next morning she came with sputum and I planned and sent it for Gen-Xpert or MTB/RIF or CBNAAT.All three are the name of same test.It is cartridge based nucleic acid amplification test.It is an automated test with negligible technician error which gives result in 2 hours. It can be done on any body fluid suspected to contain AFB(Acid fast bacillus) which is Mycobacterium tuberculosis. It is not done on blood or serum. Against the gold standard of culture, its sensitivity is 66% and specifity is 98%. Apart from detecting Mycobacterium tuberculosis, it also detects resistance to Rifampicin.,,
The CBNAAT of sputum of this child detected Mycobacterium tuberculosis along with resistance to Rifampicin.
The child was diagnosed as a case of drug resistance tuberculosis.
Drug resistant tuberculosis: it is defined as tuberculosis which is resistant to Rifampicin only.
Multi drug resistant tuberculosis:it is defined as tuberculosis which is resistant to both Rifampicin and Isoniazid.
Extented drug resistant tuberculosis:it is defined as tuberculosis which is resistant to one of the fluroquinolones and any single injectable aminoglycoside ATT other than Streptomycin in addition to Rifampicin and Isoniazid.
References:
1.World Health Organisation.Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance.XpertMTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children,policy update,Geneva,Switzerland:WHO;2013
2.World Health Organisation.Guidance for national tuberculosis programme on the management of tuberculosis in children.Geneva,Switzerland:WHO;2014