UNUSUAL MODE OF PRESENTATION OF INTRATHORACIC TUBERCULOSIS,DK JHA ,MD
Tuesday, July 19th, 2016Sania is 8 years ,female child,came to our OPD,with complaint of pain abdomen for 3-4 days.
There was no diurnal variation in pain and no relation to food intake or fasting.
The pain was not associated with vomiting or any change in bowel habit.There was no fever and no change in color or frequency of urine or burning sensation while passing urine.
The pain was not severe enough to interrupt her normal daily routine and she was attending her school as usual with no medication.
On examination,her anthropometry was appropriate for the age,general examination did not reveal any deviation from normal finding.Abdominal examination was normal,and other systemic examination was non cotributotry.
She was prescribed antihelminth in the form of Albendazole tablet, in view of high incidence of worm infestations in the area from she is coming,and pain abdomen is the usual symotom of worm infestations.
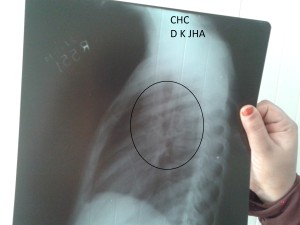
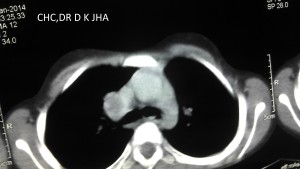
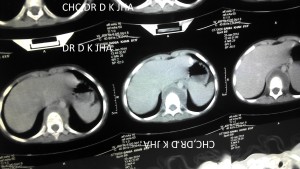
After two weeks ,she again came to OPD with pain abdomen and this time she was crying with pain since last night with vomiting tendency but no vomiting.She was admitted in general ward(Pediatrics).Symtomatic treatment was given and investigation was done to search the cause of pain abdomen. Urine and stool examination was normal.Ultrasound of abdomen showed mild enlargement of left kidney but KFT was normal.CBC did not show any marker of infection.The child was discharged as she improved clinically. She was adsviced to visit OPD with repeat ultrasound examination of abdomen after 2 weeks . She visited OPD with USG abdomen report ,which was normal this time. But the pain abdomen was persisting which was not interfering with her normal routine. After one week she came in OPD with complaint of getting difficulty in standing from sitting position.On examination there was no vertebral tenterness but the difficulty was confirmed.X-Ray thoracolumbar spine was done which was normal. Chest X-Ray was done to search the cause which revealed right hilar lymphadenopathy . Then Montoux test was done which was 22mm.GA for AFB was negative and GeneXpert test of GA did not show AFB.There was no contact history of tuberculosis. Then CECT Chest was done with contrast which revealed right hilar lymphadenopathy with central necrosis and prevertebral collection in thoracic region. The child was diagnosed as intrathoracic tuberculosis and ATT was given under CAT I and the child was responding to treatment.After 3 months of treatment the child again developed pain abdomen with vomiting.She was admitted again as oral intake was very poor.It was thought that there may be drug induced hepatitis as icterus was present and liver was enlarged and tender.Laboratory report showed s.bil 8.5 mg/dl with direct bilirubin 5mg/dl.SGPT was 1300IU/L and SGOT was 1050 IU/L.Blood was sent for viral markers and ATT was withheld.The child was improving symptomatically.The viral marker report showed Hepatitis E.Child was improved within 10 days with normal bilirubin and liver enzymes. ATT was resumed at the time of discharged and on follow up child was doing well with continuation phase of ATT which was prolonged for 2 weeks more.On completion of ATT,the child was asyptomatic,gained 3 kg weight(from 22kg to 25 kg) and repeat CXR was normal. The child is doing well in follow up for last 2 years.

SOME FACTS ABOUT TUBERCULOSIS:
- The term tuberculosis was given by Schonlein in 19th century.
- This term is derived from the English word tubercle which means lesion of consumption.
- The causative organism is mycobacterium tuberculosis which is a weakly gram positive curved rod.
- All mycobacteria form stable mycolate complexes with arylmethane dye which resist decolouration with etanol ,or any acid,so these are also known as acid fast bacilli-AFB
- Thoracic tuberculosis in children is hilar or mediastinal lymphadenitis.
- Most common type of extrapulmonary tuberculosis in children is cervical lymphadenitis.
- Common lymph nodes involved are tonsillar,submandibular,anterior cervical and supraclavicular.
- These lymph nodes enlargement should be differentiated from causes like cat scratch disease,tularemia,Brecellosis and Non mycobacterial tuberculous infections.
- Tuberculous lymphadenitis is also called Scrofula which is more common in children than adults.
- Even after proper treatment the size of lymph node may remain enlarged for months or even years.
- person having rare genetic defect of cell mediated immunity are more susceptible to this disease.
- like interleukin 12 receptor B1 deficiency and complete or partial gamma interferon receptor 1 chain deficiecy are particularly susciptable for tuberculous disease.
- Some group are specially susciptable to this disease known as Mendelian susceptibility to mycobacterial disease-MSMD
- Person having certain HLA type and containing Bcg gene are predisposed for this disease.
- This is the second most common killer infection of the world second only to HIV
- Almost one third population(2.5 billion) is infected with this disease causing organism Mycobacterium tuberculosis.
- Once infected the lifetime risk for converting into disease for an adult is 5%while in infants it is about 40% within 1 year and in children it is about 10%.
- Children in the age group of 5-15 years are relatively less sususceptible for the disease.
- Inhalation of 5-200 bacilli are needed to cause infection but even a single baicillus can cause the infection.
- one infective droplet nucleus in air contains 1-10 bacilli and its size is approximately1- 5 micron which is easily respirable and remain suspended in air for long time.
- A tuberculous nodular lesion contains 100-10000 bacilli while a cavity contains 10 million-1billion bacilli making it highly infective.
- Infection is more common at crowded place where air circulation is low.
- Infections through fomites have not been reported till now.
- Infections like measles,varicella and pertussis make the latent tuberculous infections,active.
- Children acquire the infection from adult suffering from pulmonary tuberculosis,while children to children transmission is rare because of very low bacterial load in children.
- Most common type of tuberculosis in children is intrathoracic tuberculosis.
- Most common type of intrathoracic tuberculosis in children is right hilar lymphadepathy then right paratracheal lymphadenopathy.
- Most common symptom of thoracic tuberculosis in infants are non productive cough and mild dyspnea.
- Cough may persists for few months in children even after proper treatment of reavtivation pulmonary tuberculosis.
- Fever persists for months after proper treatment of miliary tuberculosis and for weeks after proper treatment of tuberculous pleural effusion.
- Most of the adult patients of pulmonary tuberculosis become non infectios after 2 weeks of proper treatment but some may transmit disease for several weeks even on treatment.
- Once a person suffers from disease, it usually provides life time protection for subsequent disease, but second time disease has been reported in same individual.
SOME IMPORTANT TERMS USED IN CONNECTION TO TUBERCULOSIS
Exposure: This term is used when there is a definite history of contact with a person having pulmonary tuberculosis but no evidence of infection in the form of TST positive or IGRA positive
INFECTION: This term is used when there is evidence of infection in the form of positive TST (Mantoux test)or positive IGRA (Quantiferon gold)but no symptom ,no sign on clinical examination and no radiological abnormality.This is also called LTBI (Latent Tuberculous bacilli infection)
TST(Mantoux test)becomes positive after 3-12 weeks of exposure. So exposed person may be having infection even if Mantoux test or IGRA test is negative within this period.
Mantoux test is said to be positive when induration is 10mm or more.In some countries the cut off for BCG vaccinated child is 15mm.
In HIV positive children and children with severe acute malnutrition ,induration of 5 mm or more is considered positive.
IGRA(Quatiferon gold) test is not reliable below 4 years of age.
MONTOUX POSITIVE OR IGRA POSITIVE STATUS INDICATES ONLY INFECTION ,NOT THE DISEASE,WHEREASE THE NEGATIVE MONTOUX TEST DOES NOT RULE OUT THE DISEASE.
DISEASE:When there are symptoms,signs and radiological changes associated with tuberculous infection,it is called tuberculous disease and AFB may be demonstrated at this stage by various diagnostic modalities.
Only disease state is treated in India because of large prevalence of infection in this country.In western countries LTBI is also treated.
VARIOUS FORMS OF TUBERCULOSIS IN CHILDREN:
Primary pulmonary tuberculosis: This is the most common type of tuberculosis in children. In this category the bacilli enter the lung through inhalation and get lodged into lung lobe at a site just below pleura.All lung lobes are equally affected. Macrophages engulf the bacilli and cytokines released by lymphocytes attack the bacilli to kill them.There is tissue reaction and formation of epitheloid granuloma(ghons focus) and caseation at the centre of granuloma.Some bacilli which escape killing travel through lymphatics to the regional lymph nodes at the hilum.There occurs tissue reaction in the lymph nodes and its size enlarges.The enlarged lumph node along with primary focus of infection is collectively called PRIMARY COMPLEX.The enlarged lymph nodes may press the bronchus.Partial compression of bronchus causes hyperinflation of lung lobe by ball valve mechnism.When there is complete obstruction there becomes collapse of the segmental.Sometimes the lymph node erodes the bronchus and discharge caseous material into bronchus which travels to the lobe causing consolidation.Then it gives the picture of segmental collapse consolidation on chest Xray.It is also known as segmental lesion.Sometimes caseous material blocks the bronchus and causes complete collapse .Sometimes the primary infection is progressively destructive causing liquifaction of pulmonary parenchyma and then a thin walled cavity is formed. In this form of tuberculosis bullous lesion may develop which may rupture to form pneumothorax.The pathognomonic finding of this form of tubercolosis on chest Xray is relatively large size of lymph node as compared to parenchymal lesion.
Signs and symptoms are usually meagre at this stage of tuberculosis.Diagnosis is suspected by history of contact with not gaining weight or failure to thrive in an appropriate clinical setting.
Primary Progressive Pulmonary Tuberculosis: In this form, tuberculosis presents as pneumonia which may be expansile pneumonia.Signs and symptoms are prominent like bacterial pneumonia .Common symptoms are weight loss and and night sweats along with high fever and severe bouts of cough,which points towards diagnosis of Tuberculous pneumonia.,There may be lobar consolidation which may progress with caseation at the centre.It may erode the bronchus and spreads through bronchi to different areas of lungs. There may be formation of cavities when there is liquifaction of the lesion.Cavities may contain numerous bacilli which becomes dangerous to the surrounding population when there is vigourous cough.
Reactivation Tuberculosis:It occurs 1 year after primary healed tuberculous infection, when the primary sites , commonly the original primary focus,lymph node or lung apex which were seeded during primary tuberculosis reactivates due to depressed immunity of individual.Pulmonary apical seedings are known as Simons foci.It is seen usually in adults,but children rarely suffer from this form, when children acquire primary infection after 7 years of age. In this form of tuberculosis ,seen usually in adolescents, symptoms are there in the form of fever,loss of appetite,loss of weight,night sweats,cough which is productive and may contain blood in sputum,chest pain but physical signs are usually absent . Chest Xray may reveal large acinar micro nodules or large cavities which may be thick walled.This form of tuberculosis is highly contagious when there is production of large amount of sputum.
Disseminated Tuberculosis:It is the term used, when two or more organs are involved due to large numbers of bacilli released into blood stream and infecting lungs and other organs commonly liver,spleen and bone marrow.Lesions are usually large.
Miliary Tuberculosis:It is a radiological diagnosis ,when Chest Xray reveals diffuse micro nodular opacities of the size of 1-3 mm ,similar size all over the lung fields.It usually complicates the primary infection,occuring within 2-6 months of primary infection,seen commonly in infants and young children,but may be seen in older children and adults.It forms a part of disseminated tuberculosis.
WHEN TO SUSPECT A DIAGNOSIS OF TUBERCULOSIS:
- Cough for more than 2 weeks ,when common causes of cough are excluded clinically like viral upper respiratory trac infection,sinusitis,asthma,bronchiolitis
- Loss of weight of 5% or more over a period of 3 months
- Not gaining weight in a growing child
- Loss of appetite and feeling excessive tired after coming from school with no extracurricular activities.
- Fever of more than 2 weeks when common causes of fever have been excluded. Evening rise of temperature is not usually seen in children.Any pattern of fever may be present
- When pneumonia or in infants breathlessness,is not responding to standard treatment
- Contact history with adult pulmonary tuberculosis is very important point for suspicion but if clinical setting is appropriate, contact with any type of tuberculosis becomes important because sometimes pulmonary lesion remains undiagnosed.
- Period of contact for last 2 years is considered important
DIAGNOSIS:
For diagnosis, radiological examination is cornerstone.On chest Xray ,one may get hilar/mediastinal lymphadenopathy,consolidation,collapse,collapse-consolidation,cavities,fibronodular opacities,pleural effusion or pneumothorax.
TST(Mantoux test) indicates only infection so is the IGRA (Quantiferon Gold) test.
Every effort should be done to find the organism in clinically appropriate specimen.In children sputum collection is difficult so Gastric aspirate is considered a surrogate and should be examined.It should be aspirated by appropriate size Ryles tube/feeding tube in the early morning when the child is lying on the bed and has not taken orally anything in last 6 hours.After aspirating whatever quantity of gastric content, 10ml normal saline is instilled into stamach and aspirated which is mixed with previous aspirate.It is sent immediately to laboratory for smear examination. If the child is not admitted,the process can be done on ambulatory basis .Just ask the parents not to give anything orally arter midnight so that child keeps fast for 6 hours and bring the child in the morning OPD.Take GA by same process.
INDUCED SPUTUM:This is a method of collecting sputum of children who can not expectorate.Nebulize with salbutamol.Wait for 10 minutes ,then nebulize with 3% saline and do chest physiotherapy.Some children will expectorate by now. In others, aspirate the throat( Nasopharynx) by a syringe attached to feeding tube.
GenXpert test(CBNAAT): This is a method of detecting AFB in clinically relevant specimen including sputum,GA and biopsied tissue but not in blood. It has got high sensitivity and specificity and can detect Rifampicin sensitivity also.It takes 2 hours for whole process.It is available at cartain facilities in India and in private laboratory in Delhi it costs 2000-3ooo INR.
FOR SMEAR EXAMINATION FOR AFB ON MICROSCOPY ,TWO SAMPLES SHOULD BE SENT ON TWO CONSEQUITIVE DAYS ,WHEREASE ,FOR GENXPERT TEST ONLY ONE SAMPLE IS USUALLY SUFFICIENT.IF RIFAMPICIN RESISTANCE IS DETECTED ON GENXPERT THEN SECOND SAMPLE SHOULD BE SENT OR LPA TEST SHOULD BE PERFORMED WHICH ALSO DETECTS ISONIAZID RESISTANCE IN ADDITION TO RIFAMPICIN.
TREATMENT:For treatment purpose there are 2 catogaries(RNTCP INDIA)
CATOGARY 1 :New case ,smear positive or negative
CATOGARY2:Treatment after default,relapse,treatment failure and others
CATEGORY 1: Regimen 2HRZE Then 4 HRE
CATEGORY 2:Regimen 2HRZES Then 1HRZE Then 5 HRE
The prefix 2 stands for 2 months of intensive phase and 4 stands for 4 months of continuation phase in CAT 1
The prefix 2 and 1 stands for 2months and then 1 months of intensive phase and prefix 5 stands for 5 months of continuation phase in CAT 2
H-Isoniazid,R-Rifampicin,Z-Pyrazinamide,E-Ethambutol,S-Streptomycin
Daily dose is preferred over intermittent therapy.R 12-20mg/kg/day,I- 10mg/kg/day,Z-30-40mg/kg/day maximum 2.5gm /day,E-20-25mg/kg/day maximum 2gm/day,S-20mg/kg/day maximun1gm/day
CASE DEFINITION:
New case :who has never taken ATT or took it for less than 4 weeks.
Treatment after default:who has taken ATT regularly for 4 weeks and interrupted for 8 weeks and now have active disease.
Relapse:Who has taken complete trteatment and declared cure then again developed disease.
Treatment failure:who has not responded to 3 months of regular intensive phase.
In CAT1, the intensive phase can be extended for a period of one month if response is slow.The continuation phase can be extended for 3-6 months in certain clinical situation like osteoarticular and spinal lesion,meninigitis,disseminared TB and miliary TB
DRUG INDUCED LIVER INJURY(DILI) Some children may get liver injury while on intensive phase of ATT or may aquire viral hepatitis while on ATT.What to do now?
If a child develops clinical jaundice ,pain abdomen,vomiting,fever, then estimate ALT(SGPT).If it is 3 times the upper normal level or more than it,stop giving ATT for a period. Check for viral maekers for hepatitis viruses.Estimate ALT biweekly and manage the child for the condition.If the child is asymptomatic and ALT has been done to see the effect of drug on liver,then,when the level is 5 times the upper normal level or more then only hold ATT and estimate ALT biweekly.When the child is improving and ALT has come down to below 2 times the upper normal level,start with half dose Rifampicin ,give it for 3-7 days then come to full dose .Add isoniazid in half dose after 2 weeks if ALT remains low ,give it for 3-7 days then come to full dose if tolerated.Add pyrazinamide after 2 weeks if ALT remains low.ALT should be repeated twice a week during the period. If liver injury was very severe and prolonged then Pyrazinamide should not be used again.If recovry time for liver is prolonged and TB disease is life threatening the give non hepatotoxic drug like ethambutol and fluoroquinolones during recovery period.The upper normal level of ALT is 50 IU/L in children and it should be done in the morning because in the evening the value for same individual may be20- 45% more than in the morning.
PROPHYLACTIC ATT: WHO SHOULD GET IT for prevention:
- Every child below 6 years of age, in contact with smear positive adult pulmonary tuberculosis
- A child born to a mother who has been diagnosed tuberculosis during pregnancy.BCG can be given while on prophylactic ATT.
- HIV positive child if Mantoux test is 5 mm or more
- Mantoux positive child while on immunosuppressive therapy like treatment for neprotic syndrome or chemotherapy
- For prophylaxis- Isoniazid should be given in the dose of 10mg/kg/day for 6 months
- In Indian market,it is available for children as SOLONEX 100mg dispersible tablet
BEFORE STARTING PROPHYLXIS ,DISEASE SHOULD BE RULED OUT BY APPROPRIATE INVESTIGATIONS.
- Evaluation of tuberculosis diagnostics in children: 2. Methodological issues for conducting and reporting research evaluations of tuberculosis diagnostics for intrathoracic tuberculosis in children. Consensus from an expert panel.[J Infect Dis. 2012]
- A refined symptom-based approach to diagnose pulmonary tuberculosis in children.[Pediatrics. 2006]
- Intrathoracic tuberculosis in children.[Semin Respir Infect. 1996]
- Pediatric tuberculosis: problems in diagnosis and issues in management.[J La State Med Soc. 1998]
- Childhood pulmonary tuberculosis: old wisdom and new challenges.[Am J Respir Crit Care Med. 2006]
- Modifiable risk factors associated with tuberculosis disease in children in Pune, India[The international journal of tuberculosis a…]
- Towards earlier inclusion of Children in Tuberculosis (TB) drugs trials: Consensus statements from an Expert Panel[The Lancet. Infectious diseases. 2015]
- Defining the Needs for Next Generation Assays for Tuberculosis[The Journal of Infectious Diseases. 2015]
- Radiological Findings in Young Children Investigated for Tuberculosis in Mozambique[PLoS ONE. 1/01]
- Diagnosing Tuberculosis With a Novel Support Vector Machine-Based Artificial Immune Recognition System[Iranian Red Crescent Medical Journal. 1/01]


 Facebook
Facebook Twitter
Twitter Google+
Google+