Drug resistant Tuberculosis,What we know till beginning of 2021,DR.D.K.JHA,M.D.,Pediatric Pulmonologist,Delhi
Thursday, February 18th, 2021
Tuberculosis is very very old disease of human .
There has been many research in the field of diagnosis and treatment of tuberculosis.
Inspite of all the efforts worldwide,it is still the killer disease due to various reasons responsible for the emergence of drug resistant TB (Tuberculosis).
Chief responsible factors for the increased incidence of tuberculosis are poverty leading to undernutrition, and HIV infection.
Main causes of emergence of drug resistance is not completing the prescribed regimen of treatment and high burden of tuberculosis.
TERMINOLOGIES BEING USED:
Monoresistant tuberculosis-Resistance of tuberculosis to any first line drug-Rifampicin,Isoniazid,pyrazinamide,ethambutol
Polyresistant tuberculosis: Resistance of tuberculosis to more than one drug but not to both Rifampicin and Isoniazid
Multi drug resistant(MDR) tuberculosis: Resistance to both Rifampicin and Isoniazid with or without resistance to other drugs
Pre-extensively drug resistant(PRE-XDR) tuberculosis:Resistance to both Rifampicin and isoniazid with resistance to either fluoroquinilones or second line injectables but not to both fluoroquinolones and second line injectables(SLI)
Extensively drug resistant tuberculosis(XDR):Resistance to Rifampicin,Isoniazid,fluoroquinolones and second line injectables(SLI)
RR-TB:Resistance to Rifampicin with or without resistance to other antituberculous drugs
SECOND LINE INJECTABLES(SLI):Amikacin,Kanamycin and capreomycin
PRIMARY RESISTANCE:When a child or adult becomes infected with drug resistant strain of Mycobacterium tuberculosis
SECONDARY/ACQUIRED RESISTANCE:This is more common.The individual is infected with drug sensitive strain of Mycobacterium tuberculosis but it becomes drug resistant during treatment due to selection of resistant mutant strain.The cause of such resistance is incopmlete or suboptimal treatmen
TERMS USED IN DIAGNOSTIC PROCESSES
C-Tb skin test;This is a new test for the detection of tuberculosis infection.In this test ESAT6/CFP10 antigens are used.It is done in the same way as Tuberculin skin test(TST).Antigen is injected intradermally on the forearm and reaction is read after 48-72 hours with the ball pen-scale method.An induration of 5mm is taken as positive irrespective of age,BCG status and whether with HIV or non HIV.The sensitivity is comparable to TST(MANTOUX TEST) and IGRA(QUANTIFERON GOLD)
IGRA(QUANTIFERON TB GOLD IN TUBE TEST;QFT-GIT: AND T-SPOT TB TEST:T-SPOT):This test is based on the principle of white blood cells of individuals infected with mycobacterium release interferon gamma when mixed with antigens derived from Mycobacterium.In this test whole blood is taken from individual and then mixed to ESAT6/CFP10 antigens and result is available within 24 hours.It does not differentiate between active and latent Tb.This test is not affected by BCG vaccination and is specific for Mycobacterium tuberculosis but not reliable below 5 years of age.
TESTS TO DETECT MYCOBACTERIUM:
LAMP;Loop mediated isothermal amplification test is 15% more sensitive than Zeil Neilson microscopy(smear microscopy) which is most widely used traditional test to detect Mycobacterium in smear preparation of sample in the form of sputum or gastric aspirate. It is temperature independent test ,done manually for amplification of DNA and can be read by naked eye with ultraviolate light.The report is available within one hour.WHO has recommended it as an alternative to ZN microscopy as it can be used in periphery
LED-FM:Light emitting diode fluorescent microscopy is 10 % more sensitive than ZN microscopy.With proper training it can be used in periphery although its specificity is less.WHO has recommended it as an alternative to ZN microscopy.According to WHO policy paper its sensitivity is 86.3%
CBNAAT :Cartridge based nucleic acid amplification test is based on polymerase chain reaction for the ampilification of DNA.Report is available within 2 hours.It can detect live as well as dead tuberculous bacilli ,so it can not be a replacement for smear microscopy and culture based drug sensitivity test for folllow up.It is also known as GenXpert /Rif test.It also detects Rifampicin resistance.Its sensitivity is 89% and specificity is 99%
GenXpert ultra(CBNAAT ULTRA):It is an advance version of GenXpert which is ultrasensitive with main difference from GenXpert is ,it can detect Mycobacterium from sputum even if the number of bacilli per ml is as low as 16,whereas in GenXpert ,the number of bacilli should be 131/ml for detection
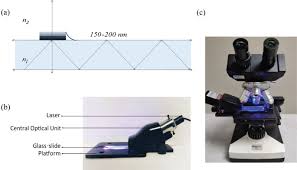
TRUENAT;It has been developed in India by Molbio Diagnostics Pvt.Ltd.Goa.Its sensitivity and specificity to detect Mycobacteria and Rifampicin resistance is similar to CBNAAT/GenXpert test.But it requires 0.5 ml of sample as compared to CBNAAT which requires 1 ml.It is battery operated and not fully automated so it does not require continuous power supply and can be used in periphery

LPA-Line probe assay is based on polymerase chain reaction with reverse hybridization technique.First line assay detects resistance to isoniazid while second line LPA detects resistance to Fluoroqinolones and SLI.Report is available within 24-48 hours.According to recent RNTCP guideline,if Rifampicin resitance is detected on CBNAAT,second sample is sent to detect isoniazid resistance by LPA.If isoniazid resistance is detected,second line LPA is done for Fluoroquinolones and SLI.If Rifampicin sensitivity is detected on CBNAAT,sample is sent for LPA to detect isoniazid resistance.
According to WHO,END TB Programme,all patients should be subjected to DST(Drug sensitivity test) and the reference standard for this test is either liquid or solid culture.The report becomes available in 12 weeks.
To meet the requirement of universal DST as recommended by WHO,rapid tests are being developed as-NEXT GENERATION SEQUENCING(NGS).It is a rapid molecular test to detect mutations responsible for drug resistance.These are of 3 types
Targeted NGS-it sequences the specific point on gene of Mycobacterium tuberculosis
Whole genome sequencing(WGS)It sequences the whole genome ,so it is better than TNGS.
Pyrosequencing-it is method of sequencing by synthesis.
DRUGS TO TREAT RESISTANT TUBERCULOSIS:
GROUP-A-Levofloxacin or Moxifloxacin,Bedaquiline,Linezolid
GROUP-B-Clofazimine,Cycloserine or Teridizone
GROUP-C-Ethambutol,Delamanid,Pyrazinamide,Imipenam-cilastin or Meropenam,Amikacin or Streptomycin,Ethionamide or Prothionamide,Para-Aminosalicylic acid(PAS)
There are TWO regimens for the treatment of drug resistant tuberculosis,Long course and Short course
Long course is for 18-20 months-According to WHO 2019 guideline, 2 drugs from Group A except Bedaquiline in children,1-2 drug from Group B along with Delamanid must be chosen and the list of at least 5 drugs is completed from Group C.After 6 months of continuation phase,Delamanid is withdrawn and at least 4 drugs should be continued for the rest of the period of treatment..
DELAMANID CAN BE GIVEN TO CHILDREN ABOVE 3 YEARS OF AGE
SHORT COURSE REGIMEN:It is given for a period of 9-12 months.Usually the intensive phase is of 4-6 months consisting of Moxifloxacin,high dose isoniazid,ethambutol,,pyrazinamide,clofazimine,ethionamide or prothionamid,Kanamycin or Amikacin(7 drugs) followed by a fixed period of 5 months of Moxifloxacin,clofazimine,pyrazinamide and ethambutol(4 drugs)
Drug resistance to Fluoroquinolones and second line injectables should be ruled out before initiating short course treatment.
Now a days it is being emphasised and WHO in June 2020 has recommended ,all oral drug regimen where injectables shuold be replaced by Bedaquiline.FDA has approved Bedaquiline above 12 years of age but in India it has been approved above 18 years in accordance to RNTCP guideline.
NOTE:High dose isoniazid- dose is 15-20 mg/kg/day-it can cause optic and peripheral neuritis,ANA positivity,agranulocytosis,vasculitis and thrombocytopenia.
Linezolid-Dose 15 mg /kg od for wt<15 kg and 10-12 mg/kg od,for >15kg.It causes Myelosuppression,peripheral and optic neuritis and lactic acidosis.It penetrates CNS well
Ethionamide/Prothionamide causes hypothyroidism
EPTB and CNS Tb should be treated with longer regimen
REFERENCES:
TB facts.GenXpert Test-TB diagnosis,TB resistance testing,CBNAAT.2018.Available at:http://www.tbfacts.org/genexpert/Accessed
2019
World Health Organisation(WHO).The use of next generation sequencing technologies for The detection of mutations Associated with drug resistance in Mycobacterium toberculosis Complex;Technical guide.Available at http://apps.who.int/iris/handle/10665/27443.Accessesd2019.
World Health Organisation.WHO consolidated guideline on Drug Resistasnt tuberculosis treatment 2019?Available at :https:apps.who.int/iris/bitstream/handle/10665/311389/9789241550529-eng.pdf.Accessed 2019
